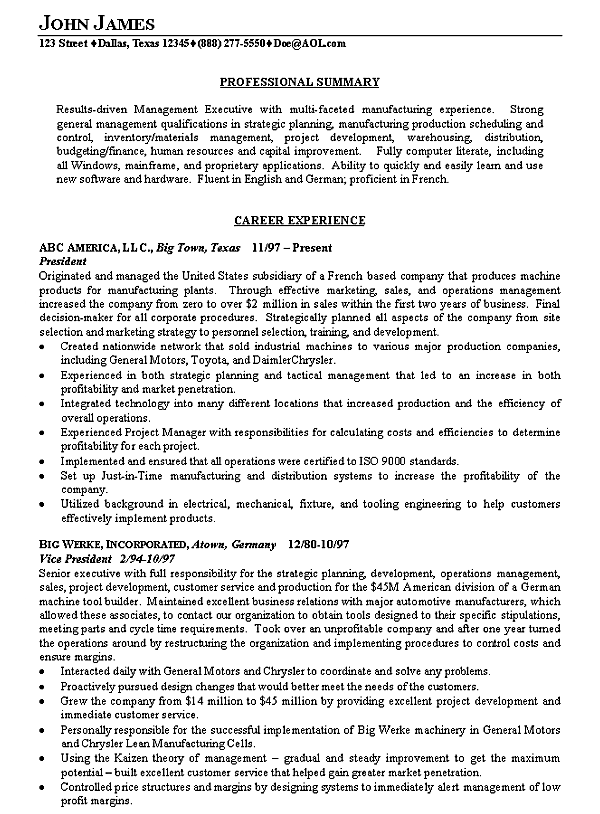
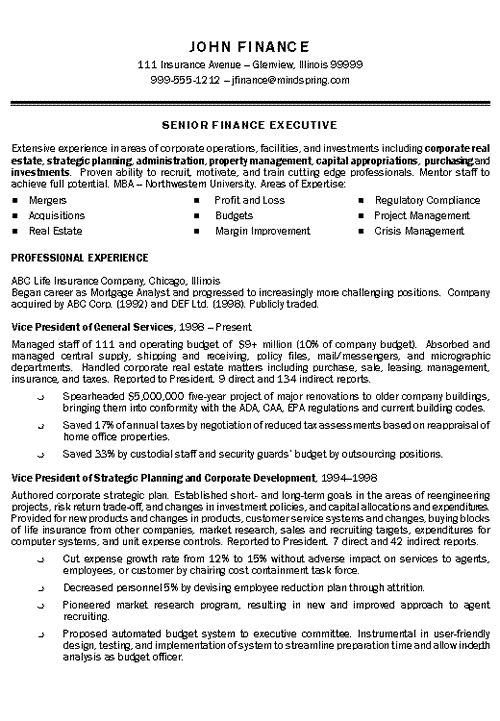
This resume was created for a financial professional that has consistently moved up the ladder at his Insurance Company. The claims analyst resume example below shows how to highlight multiple promotions within the same company.
The bullet points demonstrate that the individual was highly successful dealing with increased responsibility and workload after each promotion.
Quantifiable accomplishments were used to drive home the fact that this client has greatly improved his company’s efficiency and quality at each position.
The resume began with a Qualifications Summary specifically designed to showcase skills that are critical for positions for which he will be applying.
Also, military experience was included because it demonstrates a strong ability to lead under stressful and unpredictable circumstances.
The resume concluded with a brief section on Education because of his strong experience that was listed first on the resume.
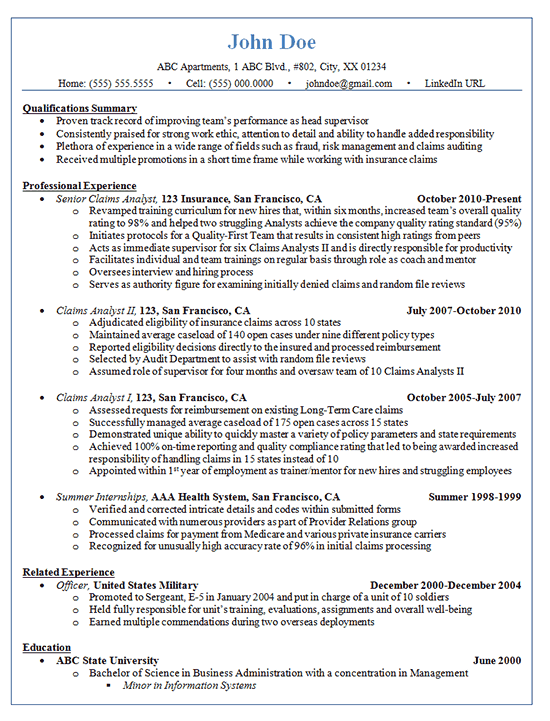
Claims Analyst Resume Example – Insurance
Claims Analyst Summary Phrases
- Proven track record of improving team’s performance as head supervisor.
- Consistently praised for strong work ethic, attention to detail and ability to handle added responsibility.
- Plethora of experience in a wide range of fields such as fraud, risk management and claims auditing.
- Received multiple promotions in a short time frame while working with insurance claims
Claims Analyst Resume Statements
- Revamped training curriculum for new hires that, within six months, increased team’s overall quality rating to 98% and helped two struggling Analysts achieve the company quality rating standard (95%).
- Initiates protocols for a Quality-First Team that results in consistent high ratings from peers.
- Acts as immediate supervisor for six Claims Analysts II and is directly responsible for productivity.
- Facilitates individual and team trainings on regular basis through role as coach and mentor.
- Oversees interview and hiring process.
- Serves as authority figure for examining initially denied claims and random file reviews.
- Adjudicated eligibility of insurance claims across 10 states.
- Maintained average caseload of 140 open cases under nine different policy types.
- Reported eligibility decisions directly to the insured and processed reimbursement.
- Selected by Audit Department to assist with random file reviews.
- Assumed role of supervisor for four months and oversaw team of 10 Claims Analysts II.
- Assessed requests for reimbursement on existing Long-Term Care claims.
- Demonstrated unique ability to quickly master a variety of policy parameters and state requirements.
- Achieved 100% on-time reporting and quality compliance rating that led to being awarded increased responsibility of handling claims in 15 states instead of 10.
- Appointed within 1st year of employment as trainer/mentor for new hires and struggling employees.